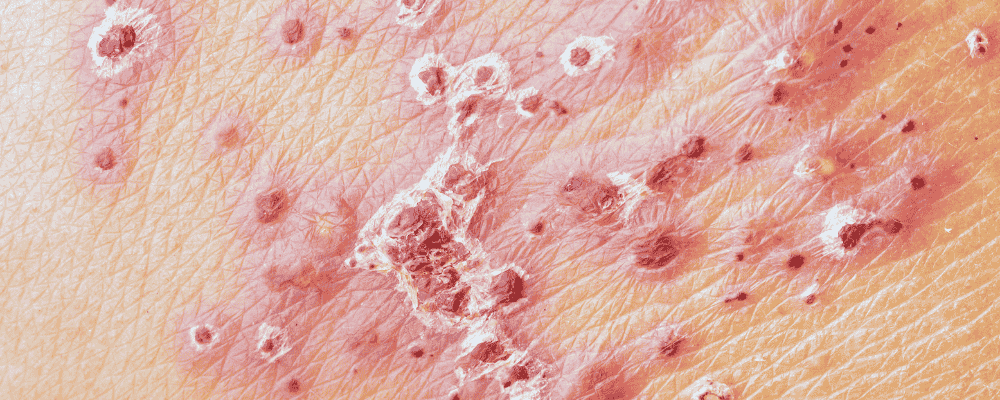
Los Angeles, 9 July — A genetically modified herpes simplex virus, RP1, in combination with nivolumab, has shown the ability to shrink and even eliminate advanced melanoma tumors—including those not directly injected—in early clinical trials. This pioneering approach in oncolytic virotherapy offers hope for patients with treatment-resistant melanoma.
In a phase 1/2 trial involving 140 patients whose melanoma had failed to respond to current immunotherapies, RP1 injections delivered every two weeks for up to eight cycles were followed by nivolumab maintenance for up to two years. Approximately one-third experienced at least 30% tumor reduction, and nearly one-sixth achieved complete remission—even in distant tumor sites not directly treated.
RP1 is a genetically engineered version of HSV‑1, stripped of genes that cause cold sores and enhanced to better infect and destroy cancer cells while activating the immune system. When combined with nivolumab—a checkpoint inhibitor that helps the immune system identify cancer cells—the therapy’s effects were amplified.
Side effects were generally mild, and the treatment was well-tolerated . Published in the Journal of Clinical Oncology and presented at the American Society of Clinical Oncology, these findings prompted the FDA to grant RP1 with nivolumab priority review. A larger phase 3 trial involving over 400 advanced melanoma patients has since commenced.
RP1 would be the second oncolytic herpes virus approved for melanoma treatment following talimogene laherparepvec (Imlygic/T‑VEC), which was first approved in 2015 for unresectable melanoma.
If FDA approval is granted, RP1 plus nivolumab could become a groundbreaking option for patients who have exhausted other treatments, offering systemic tumor regression and improved survival prospects.